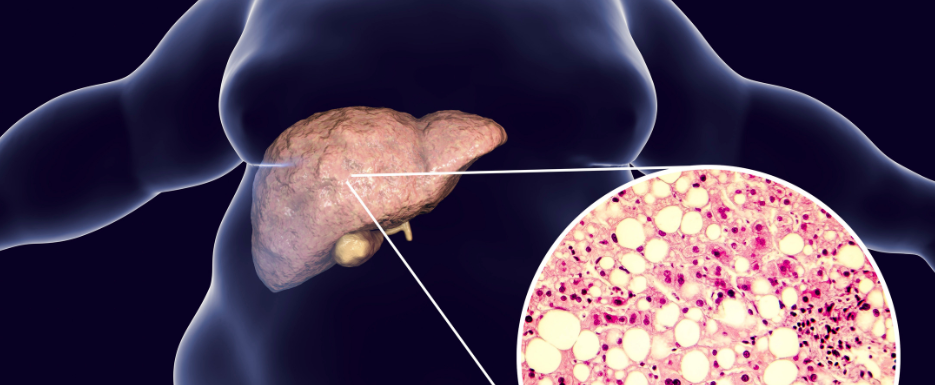
Non-alcoholic fatty liver disease (NAFLD) is the most common yet poorly investigated form of chronic liver disease, affecting over 30% of the United States population.1 NAFLD is the pathological accumulation of fat in liver cells, comprising more than 5% of the total liver weight.2
NALFD is primarily asymptomatic, and many people with NAFLD have normal liver biomarker enzymes, which leads to delays in diagnosis and a more advanced disease state before diagnosis.3,4 Adequate assessment of patients, especially those at high risk, can lead to earlier diagnosis, and the condition is reversible with proper intervention.
9 Modifiable NAFLD Risk Factors and Consequences
1. High-Fat/Carbohydrate/Fructose/Calorie Diet
The liver needs to process all the macronutrients we consume. Dietary fats and carbohydrates in excess stimulate de novo cholesterol synthesis.2,5 The newly synthesized cholesterol can cause the lipids to become congested within the hepatocytes, especially when other risk factors are present.
2. High Uric Acid
If you haven’t yet read my previous blog post on uric acid, please do so to learn about the cardiometabolic consequences of elevated uric acid levels. Uric acid is an independent risk factor for NAFLD, and high levels are associated with increased liver fibrosis.6
3. Insulin Resistance
Insulin resistance (IR) and diabetes are highly associated with NAFLD. Rates of NAFLD in people with diabetes are greater than 60%.3 Despite the high correlation, diagnosis of NAFLD is often delayed because AST and ALT levels may be normal even with increased hepatic fat content.9
IR increases liver uptake of free fatty acids and triglyceride synthesis.1 Fat deposition within hepatocytes causes an impaired liver insulin response.7 Since IR causes fatty changes in the liver and fatty changes in the liver cause IR, they are often concurrent, leading to a high association between diabetes and NAFLD. While no medications are currently approved for NAFLD, the three in consideration—metformin, pioglitazone and rosiglitazone—are all diabetes medications.2
4. Nutritional Deficiencies
Several nutritional deficiencies are associated with fatty liver development or progression. Copper deficiency promotes IR and liver steatosis—remember to always check copper-zinc ratios if recommending supplemental copper. Excessive fructose consumption inhibits copper absorption. Vitamin D deficiency is associated with IR and the progression of liver fibrosis. Low omega three fatty acids in the liver are associated with impaired fatty acid catabolism and consequential fatty acid accumulation.5 Those with NAFLD also have lower levels of vitamin E and carotenoids due to the high oxidative stress of the disease leading to antioxidant depletion and further disease progression.1
5. Mitochondrial Dysfunction
The liver is rich in mitochondria, making up a surprising 18% of total liver volume.2 Mitochondrial free fatty acid oxidation causes continuous production of reactive oxygen species. Without sufficient antioxidants, this will cause the accumulated fat to oxidize, leading to hepatocyte necrosis and collagen fibrotic deposition.1 Mitochondrial dysfunction is common in those with NAFLD, especially in older adults and those with higher adiposity or diabetes.7
6. Hypertension
People with hypertension should be screened for NAFLD because, for reasons not fully understood, the rates of NAFLD are higher than the general population at 49%. We do know NALFD can increase blood pressure by stimulating the sympathetic nervous system and the renin-angiotensin system.8,9
7. Obesity
Like IR, obesity is also highly associated with NAFLD. Concurrent disease rates between NAFLD and obesity have been up to 90% in research studies.2,4,10 In those with obesity, fatty transporter proteins are upregulated, so fatty acids are misrouted from the primary storage site (adipose tissue) to ectopic locations, like the liver and muscles.11 IR often concurs with obesity due to the secretion of adipokines and pro-inflammatory cytokines due to adipocytes altering insulin response.12
8. Hypercholesterolemia
Hypercholesterolemia is strongly correlated with the diet and IR risk factors previously discussed, excluding cases of familial hypercholesterolemia. This correlation is due to the liver’s production of cholesterol, which can become congested. High cholesterol has been associated with NAFLD at a rate of up to 90%, especially when triglycerides are elevated.9,10
9. Sedentary Lifestyle
The inclusion of sedentary lifestyle in this list should come as no surprise since diet and exercise are the two most modifiable risk factors in any cardiometabolic condition. Exercise improves insulin sensitivity, supports weight loss, and improves mitochondria size and number.2
Poorly Modifiable NAFLD Risk Factors
1. Medications
While medications can be modifiable in that there may be alternative pharmaceutical or nutraceutical interventions, they may also be the only or best option for an individual patient. Medications known to increase hepatic steatosis include corticosteroids, estrogens, methotrexate, tetracyclines, calcium channel blockers and amiodarone.6
2. Genetics
There have been associations between certain genetic mutations and an increased risk of developing NAFLD. Mutations in glycogen or lipid transporter genes, like TM6SF2, PNPLA3, NCAN and PPP1R3B, can all increase the heritability of NAFLD by up to 27%.9 This can be seen in NAFLD demographics since Black people have the lowest rates of NAFLD despite having the highest rates of obesity and diabetes. Higher rates of NAFLD are seen in those of Hispanic, Middle Eastern and Southeast Asian descent.13
NAFLD Management for Cardiometabolic Health
Resolution of NAFLD is vital as the disease can progress to cirrhosis in 4-8% or hepatocellular carcinoma in 1-5% of those affected. The most common cause of death for those with NAFLD is cardiovascular disease due to the cardiometabolic continuum of the disease process.13
Weight loss is the best option for NAFLD resolution in affected patients. Weight loss of 5-7% is sufficient to resolve NAFLD, but 8-10% is necessary for the more aggressive non-alcoholic steatohepatitis.2 A smaller portion (5-10%) of those with NAFLD are within the healthy weight range and will not require weight loss, unlike those who are overweight or obese.9
All patients can benefit from supportive interventions while working to optimize diet and exercise. The recommended interventions are located in the chart below.
| Nutrient(s) | Dose | Action |
|---|---|---|
| Bergamot and globe artichoke blend | 600 - 1,200 mg QD |
|
| Aged black garlic | 250 - 500 mg QD |
|
| Fish oil | 1,000 - 3,000 g QD |
|
| Vitamin E | 400 - 800 mg QD |
|
The Bottom Line
I hope this article has helped you understand the importance of screening your patients for NAFLD. This disease is not only underdiagnosed, but the incidence rate has continued to increase dramatically over the last few decades.9 As functional medicine providers, it is imperative that we screen patients for NAFLD—especially those who are at a higher risk of developing it—to protect their cardiometabolic health.

Megan Borreson, ND is the CM Vitals Clinical Brand Manager at Lifestyle Matrix Resource Center. She attended undergraduate school at the University of Wisconsin–Eau Claire and received her Bachelor of Science degree in cell biology and a Bachelor of Arts degree in Spanish with a minor in chemistry. Dr. Borreson then enrolled at National University of Health Sciences where she graduated summa cum laude with a Master of Acupuncture and Doctorate of Naturopathic Medicine.
References
1. Al-Busafi SA, Bhat M, Wong P, Ghali P, Deschenes M. Antioxidant therapy in nonalcoholic steatohepatitis. Hepat Res Treat. 2012;2012:947575. doi:10.1155/2012/947575
2. Ramanathan R, Ali AH, Ibdah JA. Mitochondrial Dysfunction Plays Central Role in Nonalcoholic Fatty Liver Disease. Int J Mol Sci. 2022;23(13):7280. Published 2022 Jun 30. doi:10.3390/ijms23137280
3. Fuchs M. Managing the Silent Epidemic of Nonalcoholic Fatty Liver Disease. Fed Pract. 2019;36(1):12-13.
4. Portillo-Sanchez P, Bril F, Maximos M, et al. High Prevalence of Nonalcoholic Fatty Liver Disease in Patients With Type 2 Diabetes Mellitus and Normal Plasma Aminotransferase Levels. J Clin Endocrinol Metab. 2015;100(6):2231-2238. doi:10.1210/jc.2015-1966
5. Quesada-Vázquez S, Aragonès G, Del Bas JM, Escoté X. Diet, Gut Microbiota and Non-Alcoholic Fatty Liver Disease: Three Parts of the Same Axis. Cells. 2020;9(1):176. Published 2020 Jan 10. doi:10.3390/cells9010176
6. Oral A, Sahin T, Turker F, Kocak E. Relationship Between Serum Uric Acid Levels and Nonalcoholic Fatty Liver Disease in Non-Obese Patients. Medicina (Kaunas). 2019;55(9):600. Published 2019 Sep 17. doi:10.3390/medicina55090600
7. Fromenty B, Roden M. Mitochondrial alterations in fatty liver diseases. J Hepatol. 2023;78(2):415-429. doi:10.1016/j.jhep.2022.09.020
8. Zhao YC, Zhao GJ, Chen Z, She ZG, Cai J, Li H. Nonalcoholic Fatty Liver Disease: An Emerging Driver of Hypertension. Hypertension. 2020;75(2):275-284. doi:10.1161/HYPERTENSIONAHA.119.13419
9. Iqbal U, Perumpail BJ, Akhtar D, Kim D, Ahmed A. The Epidemiology, Risk Profiling and Diagnostic Challenges of Nonalcoholic Fatty Liver Disease. Medicines (Basel). 2019;6(1):41. Published 2019 Mar 18. doi:10.3390/medicines6010041
10. Borrelli A, Bonelli P, Tuccillo FM, et al. Role of gut microbiota and oxidative stress in the progression of non-alcoholic fatty liver disease to hepatocarcinoma: Current and innovative therapeutic approaches. Redox Biol. 2018;15:467-479. doi:10.1016/j.redox.2018.01.009
11. Cobbina E, Akhlaghi F. Non-alcoholic fatty liver disease (NAFLD) - pathogenesis, classification, and effect on drug metabolizing enzymes and transporters. Drug Metab Rev. 2017;49(2):197-211. doi:10.1080/03602532.2017.1293683
12. Amor S, González-Hedström D, Martín-Carro B, et al. Beneficial Effects of an Aged Black Garlic Extract in the Metabolic and Vascular Alterations Induced by a High Fat/Sucrose Diet in Male Rats. Nutrients. 2019;11(1):153. Published 2019 Jan 12. doi:10.3390/nu11010153
13. Maurice J, Manousou P. Non-alcoholic fatty liver disease. Clin Med (Lond). 2018;18(3):245-250. doi:10.7861/clinmedicine.18-3-245