Fifty million Americans suffer from at least one autoimmune condition. Comparatively, 12 million suffer from cancer and 25 million from heart disease. This statistic cannot be explained with genetics, as genes don’t change or evolve that quickly. Rather, it points to the idea that our environment has changed drastically and is forcing us to live incongruently with that which creates health epigenetically. The current health care model is treating autoimmunity as an incurable disease whose manifestation can only be managed by suppressing the immune system. If we take a moment to consider the condition as an appropriate physiological response to environmental changes, then we will end up with an alternative protocol, one rooted in environmental changes such as diet, limited toxin exposure, sleep, exercise, and stress reduction.
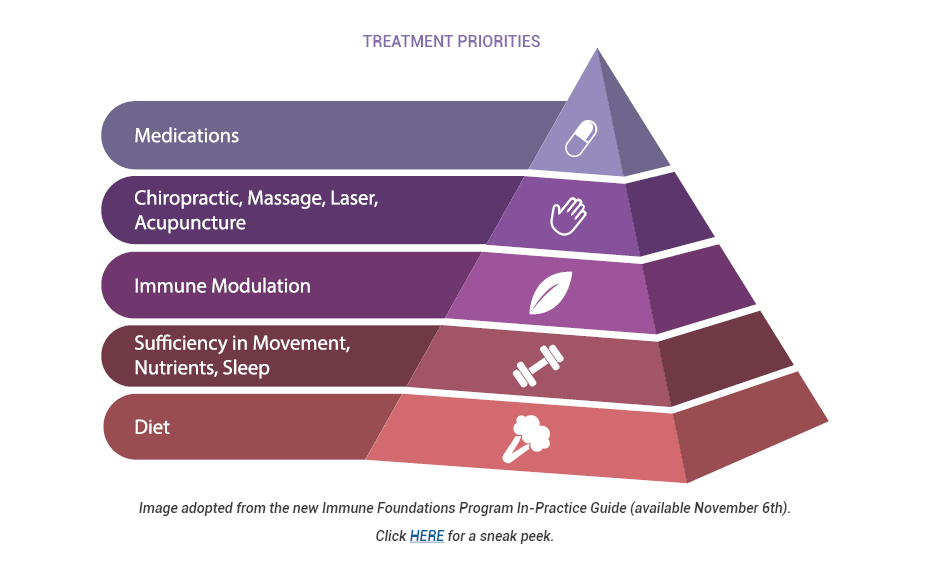
Diet
To prioritize treatment strategies for autoimmune patients, we must first consider diet. Seventy percent of the body’s immune cells live in the GI tract, and maintaining barrier function is critically important to overall health. It is impossible to optimize gut and barrier function without changing what passes through the intestinal lumen, interacts with the microbiome, and is presented to immune cells as a first line of defense. The dietary pattern chosen must eliminate foods that contribute to inflammation, such as sugar, refined grains, processed foods, and rancid fats, while also removing foods that cause intestinal permeability. These foods include dairy, gluten, sugar, and GMO varieties of plants. When these foods enter the intestines, they negatively impact the microbiome diversity and increase levels of zonulin, which regulates tight junctions between enterocytes. When these junctions are compromised, food, bacteria, medications, and toxins can enter the bloodstream and cause an immune response, which can trigger the uncontrolled production of autoantibodies.
Environmental Signals
The next layer of treatment consideration should involve environmental signals including sleep, exercise, optimal nutrient intake and absorption, and removal of toxins from the patient’s living space. The physiological inputs of these factors all impact immune system function. Maximizing sleep to at least eight hours each night is essential for cortisol levels to dip and healing to take place. Exercise should be a controlled stressor; for autoimmune patients, excessive amounts of high intensity exercise may overstress the immune system, resulting in suppression, and should be avoided. Note skincare routines, air quality, and other environmental toxins that can burden the detoxification system. This can result in endocrine and microbiome disruption. Without optimization of these lifestyle factors, the immune system will remain under stress.
Immune Modulators
In addition to diet, sleep, exercise, stress reduction, and toxin control, autoimmune patients can benefit from the use of immune-modulating herbs, nutraceuticals, ancillary therapies, and in some cases medications. However, these protocols have a much greater efficacy if the foundation of the treatment pyramid is addressed first. An initial focus on addressing lifestyle habits and barrier function will put patients on a trajectory for healing from autoimmunity.
To learn more about lifestyle and nutritional support for the autoimmune patient, attend the upcoming webinar.

Angela Lucterhand, DC
Dr. Angela Lucterhand received her doctorate in chiropractic from Palmer College of Chiropractic in Davenport, Iowa. While there, she was a graduate teaching assistant for courses including Anatomy and Physiology, Histology, the Central Nervous System, and Spinal Anatomy. She received her Bachelor of Arts at Indiana University.
Her interest in basic health care led her to become a Health Education Specialist with the Peace Corps, where she served in Mali, West Africa. Dr. Lucterhand loves teaching and was an adjunct professor for Anatomy and Physiology at Ivy Tech. Her passion in practice is addressing the root causes of disease and emphasizing the impact of lifestyle medicine.
Dr. Lucterhand practices chiropractic and functional medicine in Elkhart, Indiana, and currently holds the position of Immune Foundations Brand Manager at the Lifestyle Matrix Resource Center.