Mitochondria are often referred to as the “powerhouses” of cells and play a critical role in keeping cells healthy. As such, dysfunction of these mitochondria can be linked to nearly every chronic disease process.
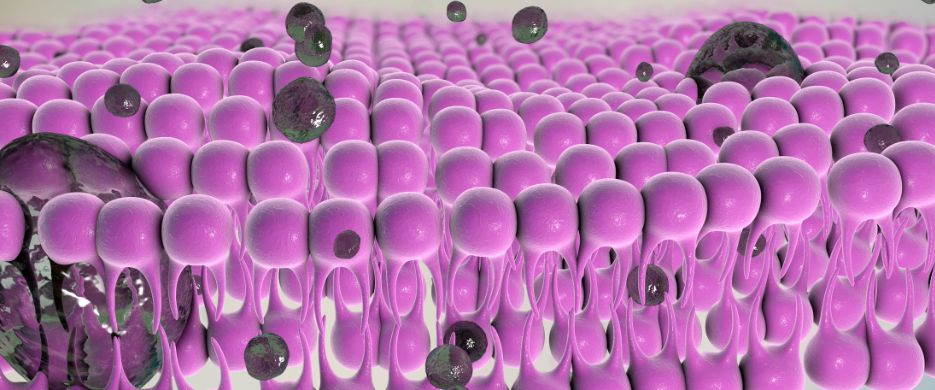
To function properly, mitochondria require a range of nutrients and compounds, including the phospholipids that make up their membranes. Phosphatidylcholine is the most abundant phospholipid in the mitochondrial membrane, making it a crucial component to keep mitochondria firing on all cylinders.1
Fatigue on the Rise
Energy levels are a growing concern across the population, given that fatigue is the most common complaint of patients seeking general medical care, and it is seen in most chronic medical conditions.2,3 Fatigue develops during aging and chronic diseases due to a variety of causes, though most notably due to loss of mitochondrial function.4,5
This loss of mitochondrial function is related to oxidative damage to mitochondrial membrane lipids.4-6 Inner mitochondrial membrane lipid damage increases proton and ion leakiness and lowers trans-membrane potential, in turn reducing the production of ATP. In chronic fatigue syndrome patients, there is evidence of oxidative damage to DNA and other biomarkers, indicating excess oxidative stress.7-10
Membrane Lipid Replacement for Fatigue
Membrane lipid replacement (MLR) is the oral supplementation of phospholipids to provide replacement molecules for membranes that are damaged during chronic illnesses, cancer and aging.11,12 Since natural phospholipid supplements are not drugs, the usual drug safety issues do not apply. Furthermore, high doses of phospholipids have been given to animals and humans over long periods without any evidence of toxic or adverse effects.12
In fact, several clinical studies have been conducted on phospholipid replacement therapy used to reduce fatigue. One study found a 40.5% reduction in fatigue—from “severe” to “moderate” fatigue on the Piper Fatigue Scale—after eight weeks of supplementation with membrane phospholipids.13
Energy Problems, Mitochondrial Solutions
When mitochondrial function is impaired, the net energy available to cells is limited, which often results in fatigue. There are several conditions and substances that can impair mitochondrial function, but peroxidation and damage of mitochondrial membrane lipids are some of the most important effects.14
The Bottom Line
Phospholipids are an essential component of healthy mitochondrial function, playing a crucial role in maintaining the integrity and fluidity of the mitochondrial membrane, protecting against oxidative stress and inflammation, and enhancing energy production. By supporting our diet with healthy supplementation of phospholipids, we can support our mitochondria and maintain optimal energy levels and overall health.
.png?sfvrsn=c0fd2cae_5)
Kareem Kandil, MD, ND is the Immune Foundations Clinical Brand Manager at Lifestyle Matrix Resource Center. Upon graduating from medical school at Ross University School of Medicine, Dr. Kandil went on to do an observership in integrative medicine and then pursued his Doctorate of Naturopathic Medicine (ND) at National University of Health Sciences in Lombard, IL.