Fifty million Americans suffer from at least one autoimmune condition. Comparatively, only 12 million suffer from cancer and 25 million from heart disease. This statistic cannot be explained with genetics, as genes don’t change or evolve that quickly. That points heavily to the idea that the environment in which we exist has changed drastically, and it is forcing us to live incongruently with what epigenetically creates health.
The current health care model is treating autoimmunity as a disease that cannot be cured, and the only way to manage its manifestation is to suppress the immune system. If we took a moment to consider the condition as an appropriate physiological response to changes in the environment, then we will end up with an alternative idea of how to correct it, which is rooted in environmental changes such as diet, toxin exposure, sleep, exercise, and stress reduction.
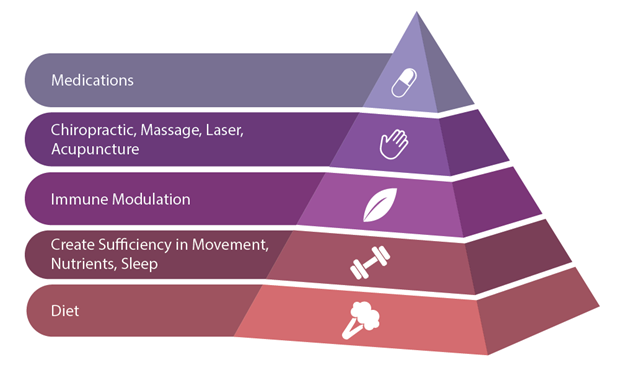
Autoimmunity Treatment Pyramid image sourced from Immune Foundations In-Practice Guide.
Autoimmunity & Diet
In order to prioritize treatment strategies for autoimmune patients, we must first consider diet. Seventy percent of the body’s immune cells live within the intestinal tract and maintaining barrier function is the first thing to address. It is impossible to optimize gut and barrier function without changing what is passing through the intestinal lumen, interacting with the microbiome, and being presented to immune cells as a first line of defense. The dietary pattern chosen must eliminate foods that contribute to inflammation, including sugar, refined grains, processed foods, and rancid fats, while also removing foods that cause intestinal permeability. These foods include dairy, gluten, sugar, and GMO varieties of plants. When these foods enter the intestines, they negatively impact the microbiome diversity and increase levels of zonulin, which regulates tight junctions between enterocytes. When these junctions are compromised, food, bacteria, medications, and toxins can enter the blood stream and cause an immune response, which can trigger the uncontrolled production of autoantibodies.
Autoimmunity & Environmental Factors
The next layer of treatment consideration should involve environmental signals like sleep, exercise, optimizing nutrient intake and absorption, and removing environmental toxins from the patients’ living spaces. These factors all have physiological inputs that impact how well the immune system functions. Maximizing sleep to a minimum of eight hours is essential for cortisol levels to dip and healing to take place. Exercise should be a controlled stressor, meaning that for autoimmune patients, excessive amounts of high intensity may overstress the immune system and result in suppression. The things patients put on their skin, breathe in the air, and encounter daily could be adding load to their detoxification systems, causing endocrine disruption, and influencing their microbiome. Without optimization of these lifestyle factors, the immune system is still under stress.
The Bottom Line
In addition to diet, sleep, exercise, stress reduction, and toxin control, autoimmune patients can benefit greatly from the use of immune-modulating herbs, nutraceuticals, ancillary therapies, and possibly medications. However, these will have much greater efficacy if the foundation of the treatment pyramid is addressed. Placing initial focus on addressing lifestyle habits and barrier function will put patients on a trajectory for healing from autoimmunity.
Dr. Angela Lucterhand received her doctorate in chiropractic from Palmer College of Chiropractic in Davenport, Iowa. While there, she was a graduate teaching assistant for courses including Anatomy and Physiology, Histology, the Central Nervous System, and Spinal Anatomy. She received her Bachelor of Arts at Indiana University.
Her interest in basic health care led her to become a Health Education Specialist with the Peace Corps, where she served in Mali, West Africa. Dr. Lucterhand loves teaching and was an adjunct professor for Anatomy and Physiology at Ivy Tech. Her passion in practice is addressing the root causes of disease and emphasizing the impact of lifestyle medicine.





