Vector of Truth: Medical Research is an Arc of Discovery
Anyone who devotes their career to scientific research is likely a seeker of truth. But this can sometimes mean taking the road less traveled. Even in medicine, it can be tempting to take the path of not seeking the hard and difficult questions about a disease, but to seek the expedient answers.
It wasn’t until recently that the connection between insulin resistance and cardiovascular disease received media attention. Historically, few in the medical community accepted the connection as plausible. In general, cardiovascular disease was seen as nothing more than a cholesterol problem.
Jeffrey Bland, Ph.D., co-founder of the Institute for Functional Medicine, and Thomas G. Guilliams, Ph.D., explain how advances in cardiovascular research have left functional medicine facing cultural obstacles, but has also created exciting opportunities for future treatments.
Be prepared for resistance to change
In 1982, doctors were still coming to terms with the idea that the origin of type 2 diabetes was not a problem with insulin inactivity as a beta cell, but over activity and resistance of the
extra pancreatic sites. At the time, linking diabetes with sugar intake was so controversial that producers escorted Bland out of a studio where Frederick Stare, MD, was speaking as part of a world tour on behalf of the Sugar Institute.
The destructive link between prominent medical researchers, like Stare, and the sugar industry recently came to light in the Annals of Internal Medicine. The public is now more aware of the fact that prominent nutritionists extolled the safety of sugar, and blamed fat as the sole cardiogenic factor in our diet under the influence of the Sugar Institute. But back in the 1980s, it was not so easy to be a truth seeker.
Even today, clinicians and researchers should be prepared to face resistance to the status quo if their research is pointing them towards a new direction. When confronted with such resistance, it can be tempting to back down completely, or to become polemic and combative against other individuals. There is always a middle path to remain in the field, so try to learn from criticism and keep marching on towards discovering truth in medical research.
The modern-day landscape of cardiovascular research is uncovering new questions about genomics, diet, and lifestyle. Researchers going down these new paths are coming from a long history of viewing cardiovascular disease as a lipid problem solved with statins. A major shift to the status quo would be to find whether statins are the answer to cardiovascular disease, or if statins are some derivative that happens to lower cholesterol.
History of the cholesterol hypothesis
Two central figures in the history of medicine played fundamental roles in determining the view on the origin of atherosclerosis. The first was Rudolf Virchow, often called the father of pathology.
His approach to his work codified the emerging science of pathology at a level that had never been known before. One of the things Virchow observed was the infrequent—during his time—cases where people died of heart attacks. During autopsies
on these patients, Virchow noticed that their coronary arteries looked like they had been abraded—as if they’d been injured. So, Virchow developed an injury hypothesis that heart disease was related to an injury of the arterial system.
Not long after Virchow developed his injury hypothesis, another important figure changed the trajectory of cardiovascular research. Nicolay Anitschkow, or Nikolay Anichkov as he is often referred, was a Russian pathologist whose animal studies largely defined future public health policy worldwide. Anitschkow ran several so-called white rabbit experiments in which he fed inbred rabbits a very high fat diet, then examined their arteries. Anitschkow found their arteries were uniformly covered in grease, and identified cholesterol as a component of the plaque in atherosclerosis. Thus, the grease-in, grease-out theory of heart disease was developed as early as 1913.
While it was true that rabbits that ate a high-fat diet ended up with fatty deposits in their arteries, research has since found some things were lost in translation with Anitschkow’s early experiments. First, the atherosclerosis Anitschkow observed in rabbits looks different to atherosclerosis in humans. Rabbits have an even deposit of plaque material across the whole arterial system. Humans, however, accumulate plaque at the bends of the arterial system. Still, the expedient explanation that eating cholesterol resulted in cholesterol deposits in arteries largely ruled the next decades of research.
Atherosclerosis research during the rest of the 20th Century was largely influenced by Ancel Keys, D. Mark Hegsted, and Dr. Frederick Stare. These researchers continued to push the idea that fat caused heart disease, with some opposing views from prominent academics, such as Dr. Jean Mayer at Tufts University.
A change in trajectory: Multiple components behind cardiovascular disease
Overtime, the idea that dietary fat caused heart disease became more complex. As more scientists studied the lipid hypothesis in different animal and human
models, it became clear that multiple other factors were associated with heart disease. For example, a chemistry analysis of the various cells found in arterial plaque, scientists realized immune dysfunction may play a role in heart disease.
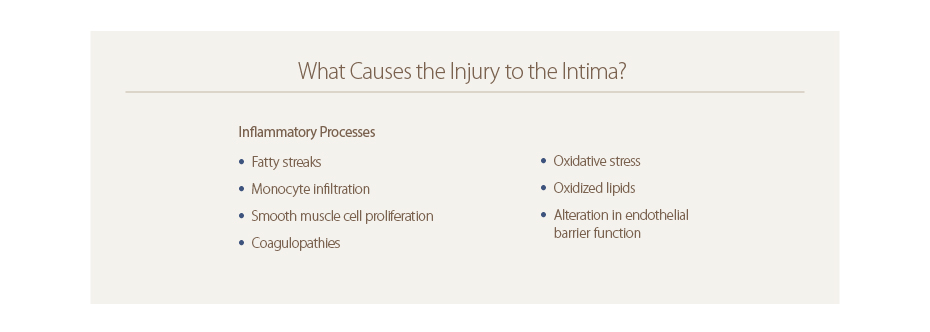
Today, several inflammatory processes have been linked to injury to the intima, the inner membrane of an artery, including monocyte infiltration, oxidative stress, and smooth muscle cell proliferation.
These discoveries complicated the view of cardiovascular disease, but they did not initially change the central thesis fighting fat fights heart disease. Anything that was a fat-buster on the molecular level, that could prevent fat from being absorbed from meals, or that would prevent biogenesis of fats was considered potentially helpful.
One large study called the Justification for the Use of Statin in Prevention: An Intervention Trial Evaluating Rosuvastatin (JUPITER) trial changed the direction of the cholesterol obsession. The JUPITER trial put patients on a controlled level of statins. However, unlike many other heart disease trials, the patients in the JUPITER trial were chosen because they didn’t have elevated cholesterol. Participants in the trial had LDL cholesterol below 120, some even below 100, and were not considered extreme examples of pathophysiological dyslipidemias.
Yet, while patients in the JUPITER trial didn’t have high cholesterol, they still saw a benefit from statins, including a significant reduction of cardiovascular incidents over a five-year period. These results introduced a whole new concept to the etiology of cardiovascular disease. If people with decent cholesterol, but a C-reactive protein test (CRP) greater than 2.0 mg/L—the cut off for health risks—saw a benefit from statins, then the JUPITER study suggests perhaps statins don’t just work via cholesterol. The JUPITER trial indicated other biomarkers, and other potential treatment targets, in cardiovascular disease.
The JUPITER trial did not upend current cardiovascular treatment overnight. Statins still generate $11 billion in annual sales, and although doctors may have assumed statins had a cholesterol-busting mechanism, statins were still proven helpful in therapy. What the JUPITER trial did shift was the direction—the curve of the arc—of cardiovascular research.
A 2016 article in the journal Cell indicated where cardiovascular research may turn in the future. The editorial, “Will Diet and Exercise Save Us All?” looked at two influential studies trying to find whether lifestyle, genes, or a combination of both determine an individual’s risk for cardiovascular disease. In short, the answer is both.
Genes or lifestyle?
One study examined in the Cell editorial was a landmark article in the New England Journal of Medicine (NEJM). In the NEJM study, researchers evaluated more than 55,000 individuals over 10 years. These study participants
were from different areas across Europe, Canada, and the United States. In addition to monitoring the health of the participants, the researchers compared the participants’ genomes to a portfolio of 80 genes associated with heart disease. The
study authors selected which genes belonged in the portfolio from a meta-analysis of other studies that examined the roughly 23,000 genes in the human genome.
Each study participant received a weighted, aggregated risk score for heart disease based on how many copies of the 80 high-risk genes they had. The participants were then placed in a low, moderate, or high- risk group based on their genetic profile. Each participant was also categorized into a low, moderate, or high-risk lifestyle group based on eating habits, exercise, obesity, and smoking habits.
The study found a healthy lifestyle couldn’t eliminate someone’s risk for cardiovascular disease if they inherited high-risk genes. Eating right and exercising could help. Patients who fell into the high-risk gene group, but had the healthiest lifestyles, had a 50 percent lower chance of cardiovascular disease than people in the high-risk gene group who led unhealthy lifestyles.
Potential in genetic analysis
With this step towards viewing cardiovascular disease as a complex, pleiotropic disease, it may soon follow that clinicians view many other chronic conditions in the same way. First, however, researchers
are going to have to analyze the human genome and compare large populations of people leading different lifestyles in different environments.
As an exercise, Dr. Bland ran an independent analysis of the 80 high risk genes included in the NEJM article’s portfolio and grouped the genes by function. The 80 genes fell into several clusters related to various functions in cardiovascular health including inflammation, lipid metabolism, vascular function, and coagulopathies. If more research refines a portfolio of high risk genes, it may one day be possible for functional medicine clinicians to do genetic screenings and direct personalized lifestyle intervention to the individual risk factors that that person has in their genes. For example, a person with a risk factor for neuropathy would need a different lifestyle intervention than someone with a lipid metabolism problem. In the future, treatments may focus on a person’s greatest genetic weak spots or uniqueness. This is a new way of thinking in healthcare, and presents a possibility for precision personalized lifestyle medicine.
Missed part 1 and part 3? Click the links below to catch up.
Part 1
Part 3
 | About Jeffrey Bland, Ph.D., FACN, CNS Jeffrey Bland is a biochemist by training, as well as a certified nutrition specialist and fellow of both the American College of Nutrition and the Association for Clinical Biochemistry. Bland served as director of nutritional research at the Linus Pauling Institute of Science and Medicine in the early 1980s, where he worked directly with Nobel laureate Dr. Linus Pauling. For more than 35 years, Bland has traveled the world teaching more than 100,000 healthcare practitioners about functional medicine. He co-founded of the Institute for Functional Medicine in 1991, and has authored several books about nutritional medicine for expert and lay audiences. In 2012, Bland founded the Personalized Lifestyle Medicine Institute (PLMI), a nonprofit organization based in Seattle, Washington, where he continues to serve as President. He is also president and CEO of KinDex Therapeutics. | |
 | About Thomas G. Guilliams, Ph.D. Dr. Guilliams earned his doctorate from the Medical College of Wisconsin (Milwaukee) where he studied molecular immunology in the Microbiology Department. Since 1996, he has spent his time studying the mechanisms and actions of natural-based therapies, and is an expert in the therapeutic uses of nutritional supplements. As the Vice President of Scientific Affairs for Ortho Molecular Products, he has developed a wide array of products and programs which allow clinicians to use nutritional supplements and lifestyle interventions as safe, evidence-based and effective tools for a variety of patients. Tom teaches at the University of Wisconsin-School of Pharmacy, where he holds an appointment as a Clinical Instructor; at the University of Minnesota School of Pharmacy and is a faculty member of the Fellowship in Anti-aging Regenerative and Functional Medicine. He lives outside of Stevens Point, Wisconsin with his wife and children. | |
Join Dr. Bland and Dr. Guilliams at the upcoming Mastering the Implementation of Personalized Lifestyle Medicine Conference!
 |
 |




